By Asenath Were
As health conditions increasingly dominate conversations at universities,according to experts, self-diagnosis and misinformation is on the rise, regarding a number of diseases, including ulcers. Dr. Geoffrey Mulindwa, the Director of Health Services at Allan Galpin Health Centre, Uganda Christian University (UCU), emphasizes that abdominal discomfort does not automatically mean
you have ulcers. “The sharing of information is now all over,” Dr. Mulindwa notes. “You can go to the internet and Google ulcers. So anybody with abdominal discomfort can claim they have ulcers, but these conditions have specific ways they are diagnosed medically.”
Dr. Mulindwa stresses that diagnosis must follow a scientific approach. Without medical evidence, assumptions about having ulcers can be misleading. “Just as the justice system demands evidence before sentencing someone, we require evidence to confirm a diagnosis,” he explains. He likens this to the “test and treat” approach used for malaria, where treatment is only administered if there is confirmed evidence of the disease in the blood or other parts of the body.
What are ulcers?
Dr. Mulindwa explains that an ulcer refers to a breakdown in the lining of any tissue, though commonly associated with the digestive system. “Ulcers can occur on the skin, in the mouth, or in the digestive tract. When people talk about ulcers, they often mean those in the stomach or duodenum,” he says. These breakdowns can range from minor irritations to larger, more serious lesions.
He uses an analogy to explain: “Think of a smooth road developing rough patches, which eventually turn into potholes. This is similar to what happens in the digestive system when ulcers form. They can occur in the stomach, duodenum, or even the intestines.”
The causes and diagnosis of ulcers
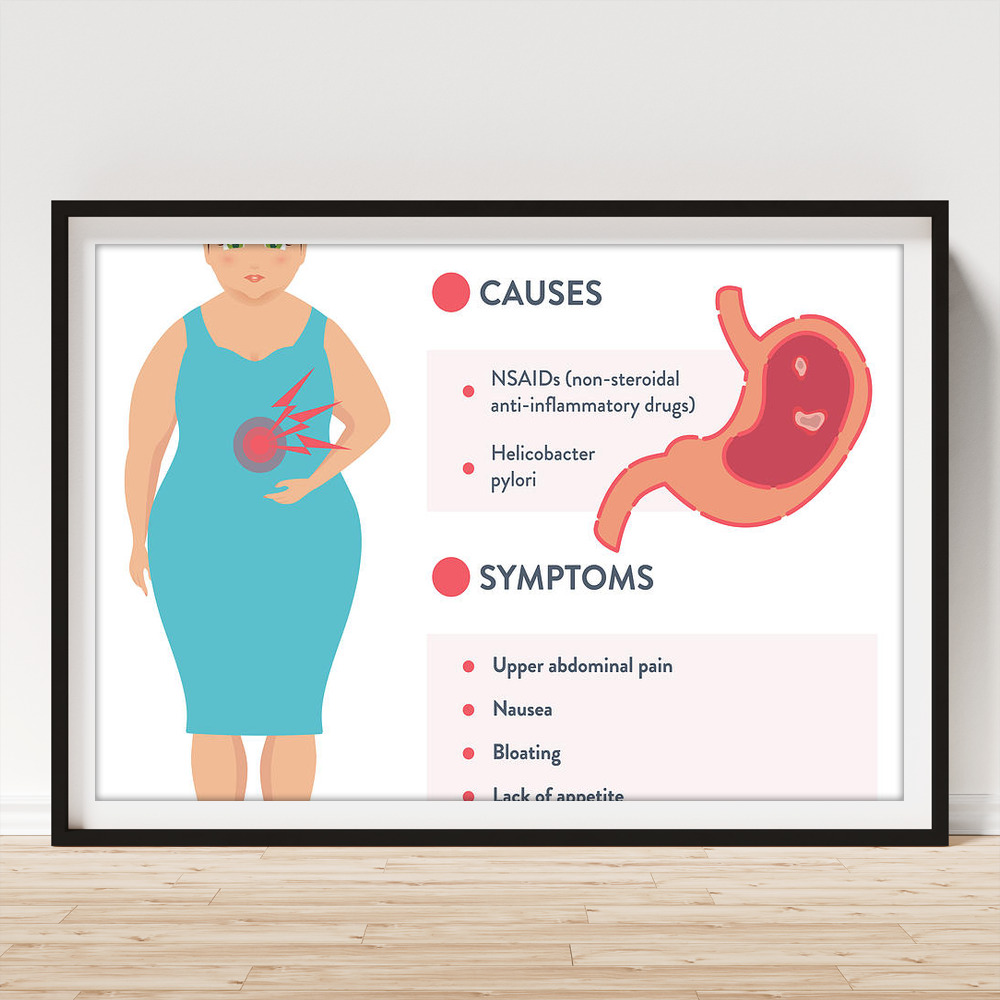
Ulcers have various causes, which means their diagnosis and treatment approaches also vary. One notorious culprit is Helicobacter pylori (H. pylori), a bacterium that erodes the stomach lining. To confirm its presence, medical practitioners rely on specialised tests.
“Another diagnostic method involves taking pictures of the digestive system lining to identify areas of breakdown. Pathologists can examine tissue samples to determine whether the ulcer is caused by conditions such as typhoid, tuberculosis, or even cancer,” Dr. Mulindwa elaborates.
Without these thorough examinations, attributing abdominal discomfort to ulcers remains speculative. “It’s not just about listening to someone say they have ulcers. Doctors must examine patients physically and conduct investigations before reaching conclusions,” he advises.
While bacterial infections like H. pylori are significant contributors, lifestyle plays a pivotal role in the development of ulcers. Dr. Mulindwa points out that peptic ulcers often result from an imbalance between high acid secretion in the stomach and low mucus lining of the stomach.
“Certain foods and habits can increase this imbalance,” he says. “Spicy foods, alcohol, nicotine, and tobacco are common culprits. Additionally, long intervals between meals or fasting can lead to low mucous levels, making the stomach lining vulnerable to acid erosion.”
Dr. Mulindwa also identifies medicines containing acids and excessive starch as potential triggers. He emphasises that listening to patients’ stories is crucial in understanding their specific circumstances and addressing their conditions appropriately.
For Grace Zawedde, a recent graduate of Journalism, Media, and Communication, ulcers were a recurring challenge during her university days. “I used to have very bad ulcers, and my doctor once told me I might need surgery,” she recalls.
Zawedde’s ulcers were made worse by a lack of proper nutrition at campus. “I think I only got ulcer attacks when I was at school because I wasn’t eating right,” she shares. “My ulcers always came along with malaria and typhoid, so it was a lot of things happening at once.”
Her turning point came when she returned home, where she had access to regular meals. “At home, food was available, unlike at campus. I started eating right, and since then, I haven’t experienced any ulcers.
Prevention and management tips
Dr. Mulindwa advises individuals with persistent or severe abdominal discomfort to seek professional medical help. “If you have discomforting pains, consult a clinical health worker. They will listen to your story, examine you physically, and conduct necessary tests,” he says.
This systemic approach ensures that treatment is tailored to the root cause of the condition. For instance, while peptic ulcers may require medications to reduce stomach acid and protect the lining, ulcers caused by infections like tuberculosis need entirely different treatments.
To prevent ulcers, Dr. Mulindwa recommends adopting healthier eating habits and avoiding triggers such as spicy foods, alcohol, and tobacco. “Ensure you eat at regular intervals to maintain a good mucus lining in your stomach,” he advises.
He also underscores the importance of managing stress and staying hydrated, as these factors contribute to overall digestive health.
While ulcers are a common health concern, proper diagnosis and lifestyle adjustments are essential for effective management and healing. As Dr. Mulindwa cautions, self-diagnosis can lead to unnecessary worry or incorrect treatments. With professional guidance and a proactive approach to health, individuals can lead ulcer-free lives and avoid the complications associated with this condition.